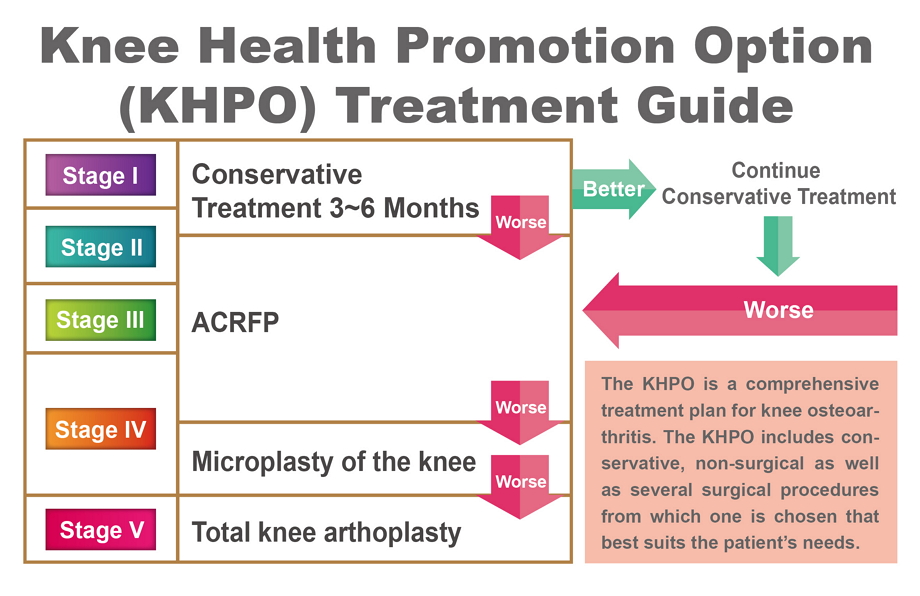
Based on our research in the medial abrasion syndrome and our expericnce in performing the ACRFP (arthroscopic cartilage regeneration facilitating procedure), we inaugurated the comprehensive Knee Health Promotion Option, KHPO, in 2007. Physicians in orthopaedics, family medicine, rheumatology, rehabilitation and their nurses are welcome to join us to provide care to sufferers of knee OA.
Unlike the well-known traditional treatments, the KHPO places its emphasis on:
We recommend that patients should, before their conditions become irreversible, undertake the arthroscopic cartilage regeneration facilitating procedure, ACRFP, which eradicates the etiological cause of their knee OA, cleans up the knee joint, and makes it hospitable to the cartilage to repair itself and then regrow. After the ACRFP, patients should strictly follow a rehabilitation routine to help themselves recover from knee OA, minimize pain, and stem the deterioration of their knee OA. Many of our ACRFP patients have seen their once-worn cartilage regrow, further improving their knee health.
This comprehensive treatment protocol includes
1.We give detailed examinations and evaluation of patient's condition and give them complete information about the protocol.
2.If necessary, we perform the ACRFP, a core component of this treatment protocol.
3.After the surgery, we accompany the patient and monitor his or her conditon regularly. The patient performs daily rehabilitation exercises as directed.
Whether a knee OA treatment plan based on the Knee Health Promotion Option (KHPO) can succeed depends above all else on the patient's understanding of and commitment to carry outing out each of the steps called for in the KHPO protocol. It is essential that the patient work closely and over a long period with the medical team to fight against this most troubling knee problem.
We offer health education and teaching videos to patients, and our case managers monitor our patients regularly to help them stay with the treatment both before and after the ACRFP surgery.
Our comprehensive treatment protocol for knee OA is based on a completely new theory that focuses on the eradication of risk factors for knee OA and on the facilitation of cartilage regrowth.
Based on this new clearly laid-out theory, our treatments, such as Arthroscopic Medial Release (AMR), Arthroscopic Cartilage Regeneration Facilitating Procedure (ACRFP), and Knee Health Promotion Option (KHPO), have been proved to be effective in a clinical setting as evidenced in our post-operative follow-ups on thousands of patients.
Therefore, our arthroscopic treatments are vastly different from and superior to the traditional arthroscopic surgery, which lacks theoretical benefits and results in varied, unpredictable levels of clinical benefits.
We will discuss each of the steps in the Knee Health Promotion Option (KHPO) in turn. When you have finished reading this discussion, you will understand how to use your knees correctly. If you should experience knee problems, you will know how to self care before seeing a doctor and avoid doing things unwittingly to hurt your knees.
Before a new patient start to undergo the KHPO treatment plan, we thoroughly examine him or her condition, including his or her X-rays in three positions: standard AP (standing anterior-posterior), lateral, and supine bent knee.
Joint space, bone spurs, femoral-tibial angle, and joint stability are assessed. Each of the three articular cavities is examined and clinically staged individually. The most advanced stage of the three is used as the stage of that knee. Our experience over many years has shown that this method of staging has been a reasonable predictor of the actual condition in the knee when we examine it through arthroscopy.
Table 1 By knee OA stage (of a medial lateral cavity), typical signs seen on X-rays and through arthroscopy
| stage | Joint space narrowing | Bone spurs | Femoral-tibial angle | stability | Arthroscopic observation |
| I | suspect | no | normal | normal | Smooth surface but losing elasticity |
| II | No more than 1/2 | suspect | >0 | normal | Rough surface and mild abrasion on the cartilage(protruding, fibrotic surface, ) |
| III | Marked, more than 1/2 | yes | Close to 0 | normal | Severe abrasion on the cartilage (fractured cartilage, the bone underneath the cartilage is less than ½ exposed) |
| IV | No space | marked | <0 | normal | The entire layer of cartilage is worn (the bone underneath the cartilage is more than ½ exposed ) |
| V | No space | marked | Severe deformity | Loose,unstable | The cartilage is entirely worn out |
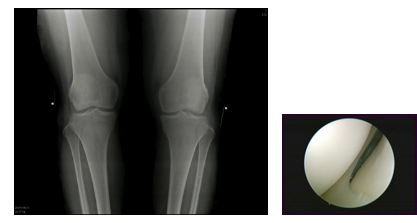
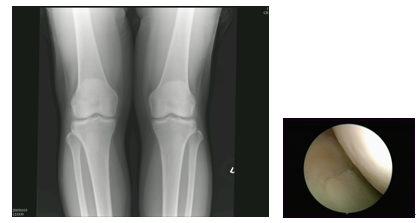
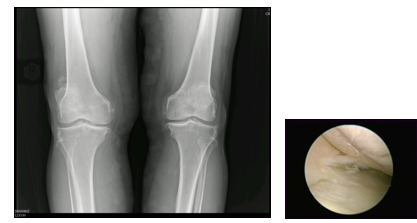
The following shows OA knee joints in X-ray and arthroscopy through the stages of deterioration:
Normal: Normal knee joint space in X-ray and smooth and shiny cartilage surface in arthroscopy
Stage I: Normal knee joint space in X-ray, cartilage surface in arthroscopy has become less smooth and shiny.
Stage II: Narrowed knee joint space in X-ray, In arthroscopy, the shine on the cartilage surface has disappeared, local bumpy spots have become visible, and the cartilage has become less elastic.

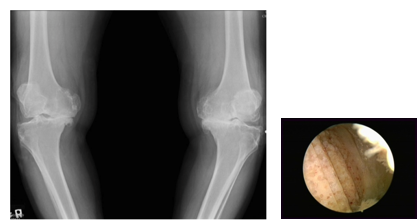
Stage III: Even more narrowed knee joint space in X-ray, In arthroscopy, the cartilage surface has crumpled or abraded, appearing whisker-like.
Stage IV: The joint space is almost all gone and bone spurs are obvious. In arthroscopy, some cartilage is completely worn off, and the bone underneath is exposed.

Stage V: The joint space is all gone and bone spurs are obvious. In arthroscopy, all cartilage is completely worn off. Severe deformity has led the lateral ligament to become loose, unable to provide stability.
We recommend that all stages I and II and certain stage III patients undertake conservative treatment under medical supervision for at least three months. The patients and their families must completely understand the reasoning behind the conservative treatment in order for it to be successful.
We first emphasize that medial abrasion phenomenon is an important cause for osteoarthritis. Then we review the daily routine of a patient so we may discuss how, if anything, to modify his or her routine at home, on the job, or during workouts so as to minimize abrasion in his or her knee. In principle, movements that require repeated bending of the knee are harmful to the knee.
Table I is compiled based on this principle, Therefore, if your activity is not on this list, you can apply this principle to judge if it is knee friendly.
To avoid exerting shearing force harmful to cartilage regeneration, a recuperating patient should avoid repeatedly bending their knees more than 50 degrees. Therefore, sufferers of OA knees may engage in activities such as walking, jogging, golfing, and swimming freestyle or butterfly strokes. But they are advised to refrain from knee-damaging activities such as climbing up or down stairs, mountain climbing, squatting (such as gardening), bicycling, and swimming breaststroke.
Three recommended rehabilitation exercises under the KHPO
Like tooth brushing for oral hygiene, these rehabilitation exercises are recommended to be performed lifelong for the health of your knee.
| Suitable activities | Harmful activities |
| Walking | Climbing up or down stairs |
| Jogging | Mountaineering |
| Golfing | Repeatedly Squatting or kneeling (e.g. Gardening) |
| Freestyle swimming | Bicycling |
Patients are advised to work closely with our trained staffers, such as case manager or nurse, to monitor their adherence to and progress in their at-home rehabilitation regimens, which often include exercises to strengthen muscles around the knee and to stretch soft tissues.
Once we have staged a knee, we advise the patient to undergo a conservative treatment of exercises to strengthen and stretch out his or her quadriceps and soft tissues, respectively. We also advise the patient of the potential surgery, based on Table 3, that he or she may possibly be receiving.
For stages I, II, and III patients, Arthroscopic Cartilage Regeneration Facilitating Procedure (ACRFP) is a better treatment than knee replacement. For stage IV patients, knee replacement is typically the first choice, but when certain conditions exist, the ACRFP could be a very good choice.
| Stage | ACRFP | Microplasty of the knee | TKA (total knee arthroplasty) |
| I | + | - | - |
| II | ++ | - | - |
| III | +++ | ++ | - |
| IV | + | +++ | ++ |
| V | - | + | +++ |
In 2005, we developed a novel surgical procedure Arthroscopic Medial Release (AMR) to treat the medial abrasion syndrome.
As early as 1940, surgeons already severed the medial collateral ligament of the knee to treat knee OA with severe deformity, and papers were first published in 2001 about arthroscopic surgery to severe medial collateral ligament of the knee to treat knee OA. They attributed the therapeutic benefits simply to the reduction of pressure. However, those benefits did not last long and those arthroscopic surgeries did not catch on because those physicians did not know about the medial abrasion phenomenon which is an important cause of knee OA.
Unlike those arthroscopic procedures that merely severed the medial ligament indiscriminately, our Arthroscopic Medial Release procedure is precisely targeted to sever the third layer and a small part of the second layer (see the diagram) of the three-layer medial support structure in the knee.The capsulectomy extends superiorly to the midline of suprapatellar pouch. Inferiorly, it extends to the upper margin of medial meniscus. Anteriorly, it extends to the medial margin of patella. Posteriorly, it is undertaken to remove portion of the conjoined part of layer II and III till the gracilis tendon is visualized. Only the deep medial ligament was severed by this procedure and the medial stability should not be disturbed much.
Because only the deep medial ligament is severed, this procedure does not impact the stability of the knee.
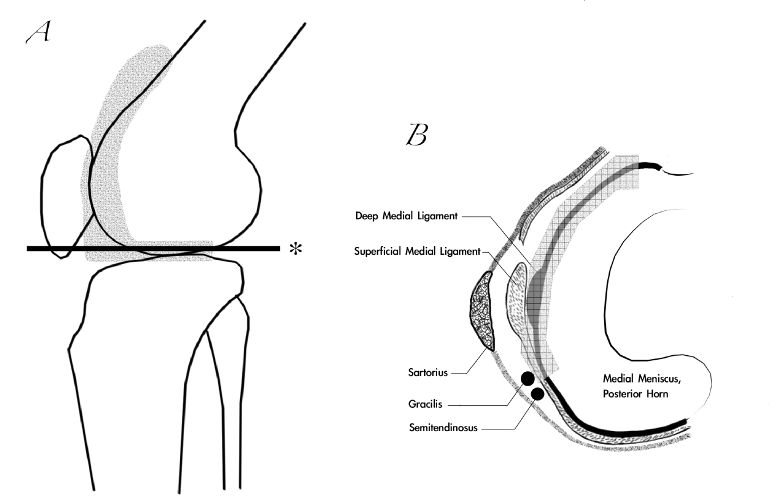
Diagram A: The shaded area is the area excised in an AMR operation.The extent of the medial capsulectomy is shown in the hatched area of the line drawing of the lateral view of the knee joint. The line marked by * is the level of crosssection above the meniscus as shown in Diagram B.
Diagram B: The arrowed area indicates the extent of the capsulectomy above the medial meniscus. Note that only the deep medial ligament is severed. The tendon of gracilis could be visualized after the procedure.
The adequacy of the medial release could be checked by passing the scope under the patella and verified if the previously tightly closed medial patellofemoral joint space could be easily opened and the medial retinaculum visualized when the knee was put in full extension position.
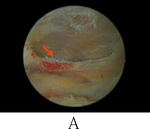

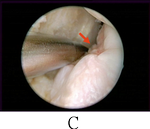
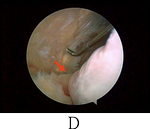
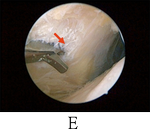
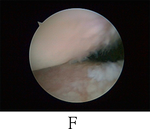
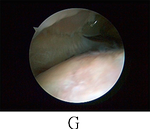
For a complete arthroscopic medial release (MAS), A, proximally, the genu articularis muscle attachment (arrow) should be released; B, the anterior synoviomeniscal junction (arrow) should be release; C, the medial gutter should be cleared to its posterior corner (arrow); D, the synoviomeniscal junction of the medial meniscus (arrow) should be clearly seen; E, in some case, release of the fascia of pes anserinus (arrow) should be performed; F, before medial release; G, after medial release.
According to our experience of performing this procedure (Lyu SR, 2008), the outcome of
255 knees in 173 patients for varying stages of osteoarthritis involving the medial compartment supports our contention that AMR is a good modality for the treatment of osteoarthritis of the medial knee joint in the aspect of symptom relief. It can reduce the pain
in the majority of OA patients over a period of at least 4 years. In some cases, we also found the evidence that AMR could modify the disease process and satisfied the patients.
The clinical outcome of the AMR led us to believe that, by eradicating the abrasion phenomenon between the tight, fibrotic and hypertrophied medial plica related structure and the opposite medial femoral condyle, the pain of most patients could be reduced and the degenerative process in the medial compartment of some patients might be decelerated
or arrested. Therefore, we propose a concept of arthroscopic cartilage regeneration facilitating procedure (ACRFP) that combines arthroscopic medial release (AMR) with synovectomy, abrasional chondroplasthy, partial meniscectomy or percutaneous lateral
release (PLR) as a rationale for the deliberate arthroscopic management of OA knee. We believed that the elimination of the detrimental factors including the medial abrasion phenomenon, focal or generalized synovitis, chondral flaps, meniscus flaps or lateral compression phenomenon will provide a more hospitable environment for the damaged cartilage to regrow.
The ACRFP is built on a clear theoretic foundation and proven clinically. Its primary clinical objectives are
1.to remove all abnormal frictions, such as collagen fragments from damaged cartilage, and pinching phenomena, such as inflamed and thickened synovium, in the knee,
2.adjust and release excessive tension between articular surfaces as a result of repeated inflammation of soft tissues over a long period so as to relieve articular surfaces of harmful pressure,
3.remove all inflamed and thickened synoyium in the knee, which may cause cartilage to breakdown.
Proper execution of the ACRFP can improve the environment in the knee, making it more hospitable for cartilage to repair itself naturally.
Our surgical experiences, X-rays, and long-term follow-ups of patients have enabled us to be certain of this conclusion:
The ACRFP is an effective treatment for knee OA and it improves the course of this common disorder. If the existing catabolic factors in the knee joint have been thoroughly removed—which the KHPO does—the anabolic factors begin to take the lead in repairing the damaged knee. Then the damaged cartilage can regenerate and repair itself.
After the detrimental factors including medial abrasion syndrome, lateral compression syndrome, synovitis, chondral debris and meniscus flaps that have been proven as the main causes of cartilage damage are eliminated by ACRFP, the purpose of the post-operative care is to unveil and facilitate the natural repairing ability of the degenerated cartilage. During the first 3 months after ACRFP, the aim of rehabilitation is to prevent scar contracture and consequent recurrent medial abrasion phenomenon. Gentle deep bending stretching exercise is encouraged after each session of quadriceps strengthening exercise. To facilitate cartilage regeneration, strict rules about engaging into appropriate daily activities and exercises as listed in table 3 should be followed during the first post-operative year. The rationale of this precaution is to avoid repeated bending of the knee that might produce shearing force harmful for cartilage regeneration. Patients are advised to do muscle strengthening and soft tissue stretching exercises around the knee for as long as possible.
The PCRFM includes:
1.Rehabilitation exercises. These are the most economical and efficient method.
(1)the exercise to strengthen the quadriceps by extending the leg (diagram A).
(2) During the three months after the ACRFP, the objectives of rehabilitation is to prevent scarring on the wound, which could bring about the recurrence of the medial abrasion phenomenon, Therefore, each time after you have finished your quadriceps exercise, you must also do both press knee, (B), and knee hug, (C).
(3)To promote cartilage regeneration, you are advised to observe and do only exercises that are listed in Table 3, exercises that do not bend the knee repeatedly and possibly create frictions that hinder the re-growth of cartilage. Walking is the most convenient and effective exercise. It also helps keep your weight down.
(4)One year after the ACRFP, if appropriate, you may gradually return to your own original routine.
(5)These three exercises help prevent cartilage from being damaged again. Therefore, if at all possible, you are advised to keep doing them forever.
 |
 |
 |
| A. "Leg Raise" for quadriceps strengthening Objective: to strengthen and keep the endurance of your thigh muscle |
B. "Knee Press" for anterior soft tissue stretching Objective: to maintain appropriate tension between cartilage |
C. "Knee Hug" for posterior soft tissue stretching Objective: to maintain appropriate tension between cartilage |
2.Medical establishments elsewhere have promoted external therapies that claim to stimulate the growth of cartilage. These methods are more costly but offer uncertain results. Some studies have shown these methods to suppress inflammation, and PRP has been shown to facilitate the anabolism of cartilage and enhance its ability to repair itself. Perhaps they deserve a closer look.
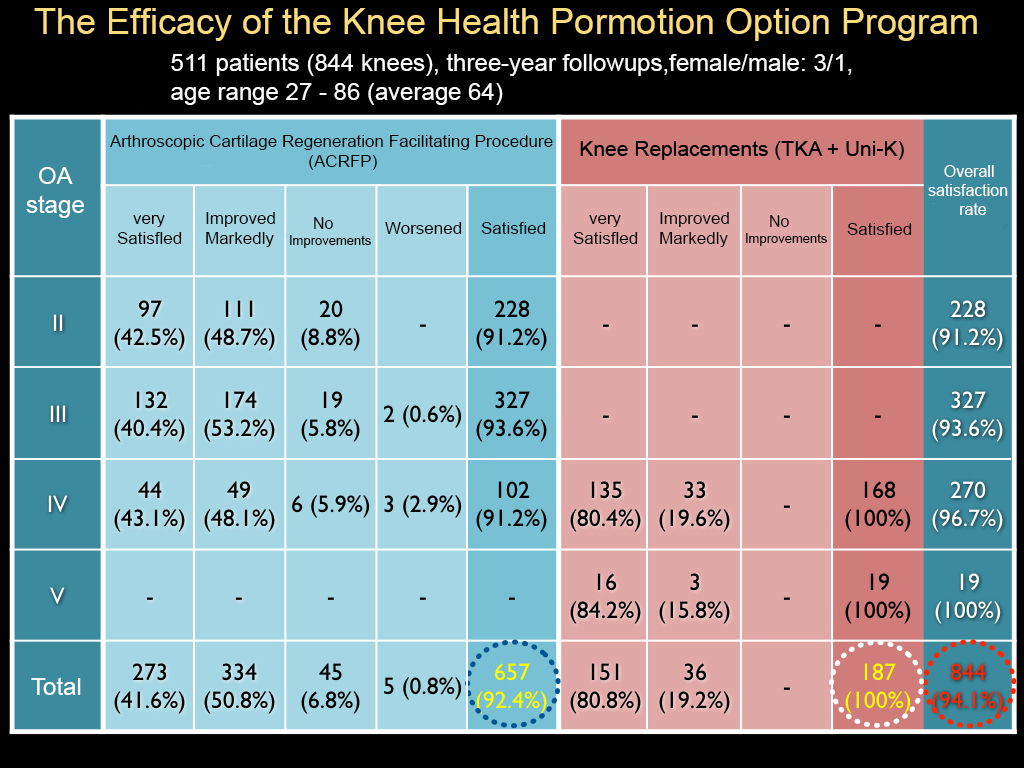
[/hide]Overall, 94.1 percent of our patients have been satisfied with the KHPO
After one year, 511 patients with 844 affected knees (97.9%) remained enrolled in the study. The mean age of these patients at the time of surgery was 64 years (SD: 10). Subjective assessment was satisfactory in 794 (94.1%) knees. Six-hundred-and-fifty-seven knees (77.8%) of 379 patients received an arthroscopic cartilage regeneration facilitating procedure (ACRFP), 71 knees (8.4%) of 70 patients received unicompartmental arthroplasty (UKA), and 116 knees (13.8%) of 116 patients received total knee arthroplasty (TKA). For the arthroplasty group, the subjective assessment was satisfactory in 187 knees (100%). For the ACRFP group, the subjective assessment was satisfactory in 607 knees (92.4%). In the ACRFP group, the satisfactory rate was 91.2% for 228 stage II knees, 93.6% for 327 stage III knees, and 91.2% for 102 stage IV knees. Three knees in the stage IV group had converted to arthroplasy after the minimum follow-up of one year.