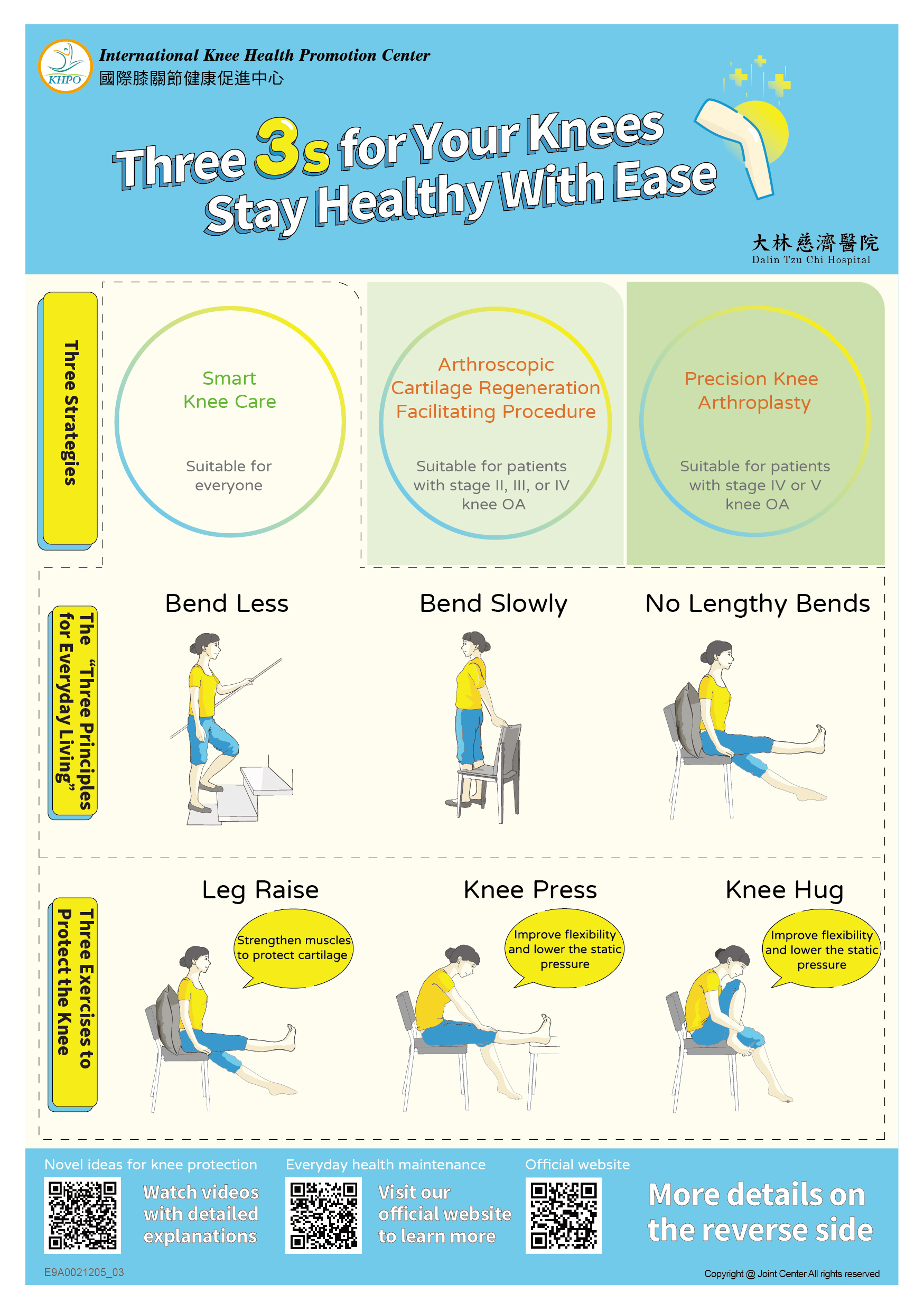
Based on our research in the medial abrasion syndrome and our expericnce in performing the ACRFP (arthroscopic cartilage regeneration facilitating procedure), we inaugurated the comprehensive Knee Health Promotion Option, KHPO, in 2007. Physicians in orthopaedics, family medicine, rheumatology, rehabilitation and their nurses are welcome to join us to provide care to sufferers of knee OA.
Unlike the well-known traditional treatments, the KHPO places its emphasis on:
We recommend that patients should, before their conditions become irreversible, undertake the arthroscopic cartilage regeneration facilitating procedure, ACRFP, which eradicates the etiological cause of their knee OA, cleans up the knee joint, and makes it hospitable to the cartilage to repair itself and then regrow. After the ACRFP, patients should strictly follow a rehabilitation routine to help themselves recover from knee OA, minimize pain, and stem the deterioration of their knee OA. Many of our ACRFP patients have seen their once-worn cartilage regrow, further improving their knee health.
This comprehensive treatment protocol includes 1.We give detailed examinations and evaluation of patient's condition and give them complete information about the protocol. 2.If necessary, we perform the ACRFP, a core component of this treatment protocol. 3.After the surgery, we accompany the patient and monitor his or her conditon regularly. The patient performs daily rehabilitation exercises as directed.
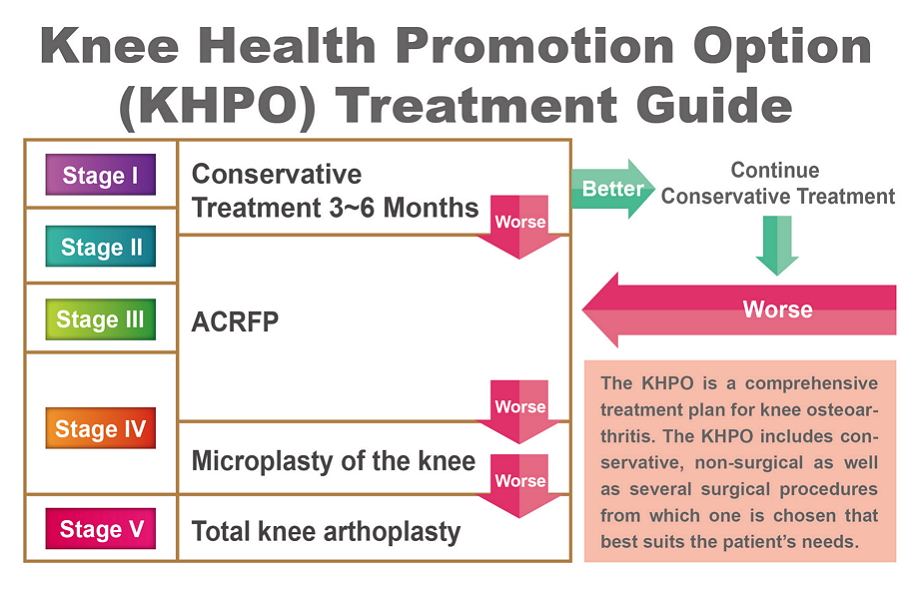
Knee Health Promotion Option (KHPO) Treatment Guide
The KHPO is a comprehensive treatment plan for knee osteoarthritis. The KHPO includes conservative, non-surgical as well as several surgical procedures from which one is chosen that best suits the patient’s needs.
Whether a knee OA treatment plan based on the Knee Health Promotion Option (KHPO) can succeed depends above all else on the patient's understanding of and commitment to carry outing out each of the steps called for in the KHPO protocol. It is essential that the patient work closely and over a long period with the medical team to fight against this most troubling knee problem.
We offer health education and teaching videos to patients, and our case managers monitor our patients regularly to help them stay with the treatment both before and after the ACRFP surgery.
Our comprehensive treatment protocol for knee OA is based on a completely new theory that focuses on the eradication of risk factors for knee OA and on the facilitation of cartilage regrowth.
Based on this new clearly laid-out theory, our treatments, such as Arthroscopic Medial Release (AMR), Arthroscopic Cartilage Regeneration Facilitating Procedure (ACRFP), and Knee Health Promotion Option (KHPO), have been proved to be effective in a clinical setting as evidenced in our post-operative follow-ups on thousands of patients.
Therefore, our arthroscopic treatments are vastly different from and superior to the traditional arthroscopic surgery, which lacks theoretical benefits and results in varied, unpredictable levels of clinical benefits.
We will discuss each of the steps in the Knee Health Promotion Option (KHPO) in turn. When you have finished reading this discussion, you will understand how to use your knees correctly. If you should experience knee problems, you will know how to self care before seeing a doctor and avoid doing things unwittingly to hurt your knees.
Before a new patient start to undergo the KHOP treatment plan, we thoroughly examine him or her condition, including his or her X-rays in three positions: standard AP (standing anterior-posterior), lateral, and supine bent knee.
Joint space, bone spurs, femoral-tibial angle, and joint stability are assessed. Each of the three articular cavities is examined and clinically staged individually. The most advanced stage of the three is used as the stage of that knee. Our experience over many years has shown that this method of staging has been a reasonable predictor of the actual condition in the knee when we examine it through arthroscopy.
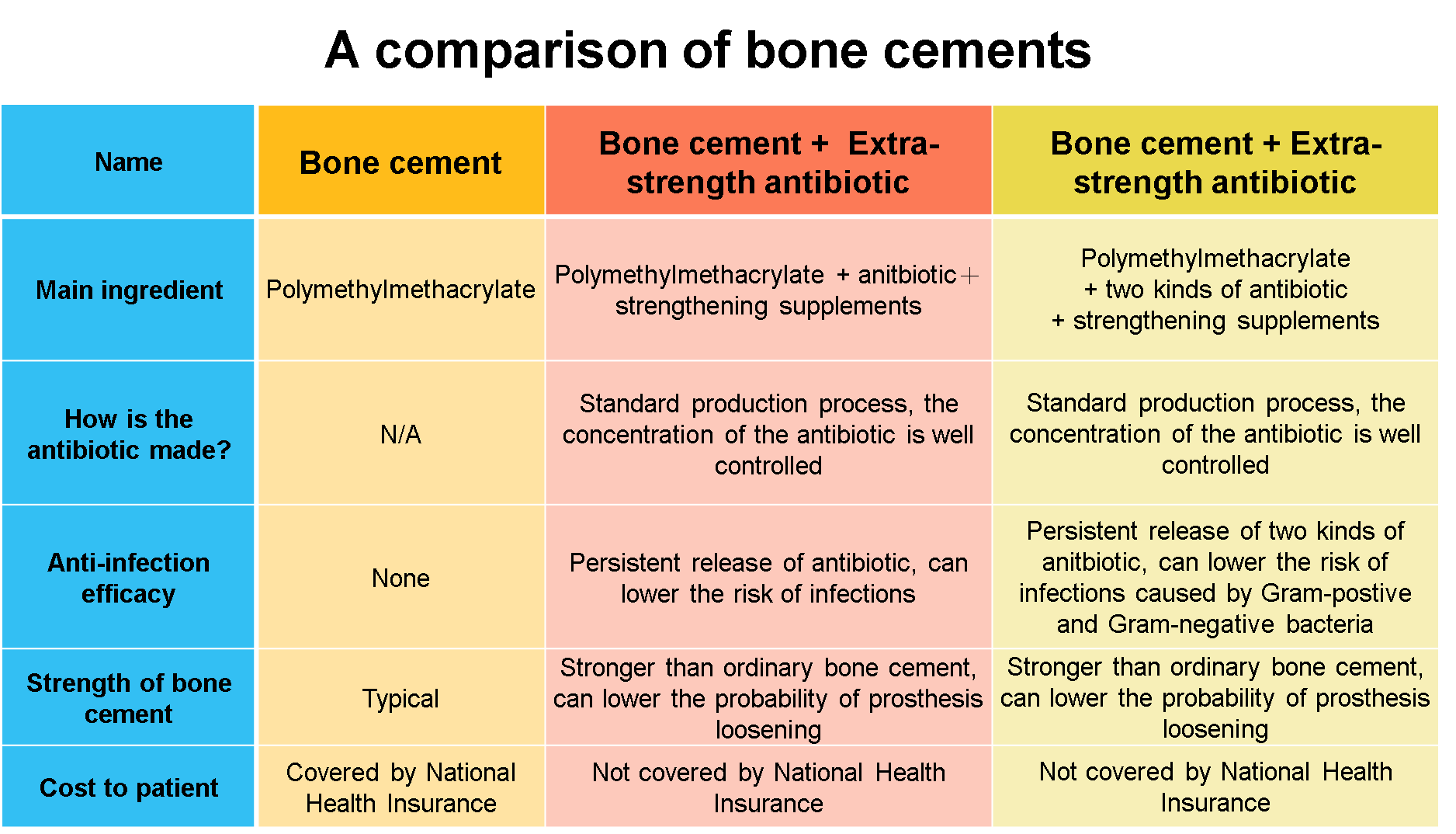
Table 1 By knee OA stage (of a medial lateral cavity), typical signs seen on X-rays and through arthroscopy
| stage | Joint space narrowing | Bone spurs | Femoral-tibial angle | stability | Arthroscopic observation |
|---|---|---|---|---|---|
| I | suspect | no | normal | normal | Smooth surface but losing elasticity |
| II | No more than 1/2 | suspect | >0 | normal | Rough surface and mild abrasion on the cartilage (protruding, fibrotic surface, ) |
| III | Marked, more than 1/2 | yes | Close to 0 | normal | Severe abrasion on the cartilage (fractured cartilage, the bone underneath the cartilage is less than ½ exposed) |
| IV | No space | marked | <0 | normal | The entire layer of cartilage is worn (the bone underneath the cartilage is more than ½ exposed ) |
| V | No space | marked | Severe deformity | Loose,unstable | The cartilage is entirely worn out |
The following shows OA knee joints in X-ray and arthroscopy through the stages of deterioration:
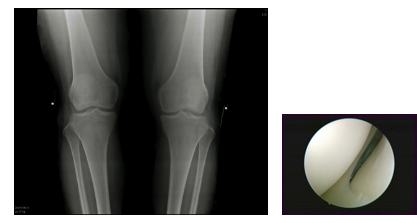
Normal:
Normal knee joint space in X-ray and smooth and shiny cartilage surface in arthroscopy
Stage I:
Normal knee joint space in X-ray, cartilage surface in arthroscopy has become less smooth and shiny.
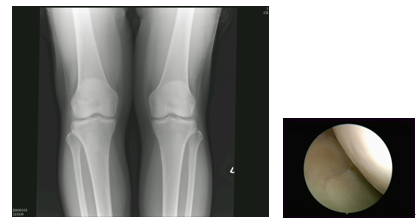
Stage II:
Narrowed knee joint space in X-ray, In arthroscopy, the shine on the cartilage surface has disappeared, local bumpy spots have become visible, and the cartilage has become less elastic.
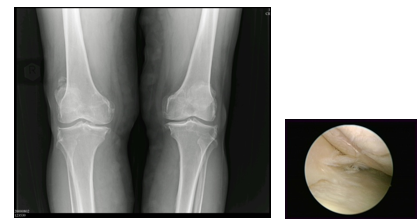
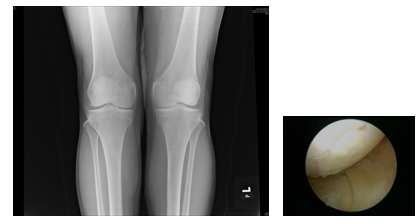
Stage III:
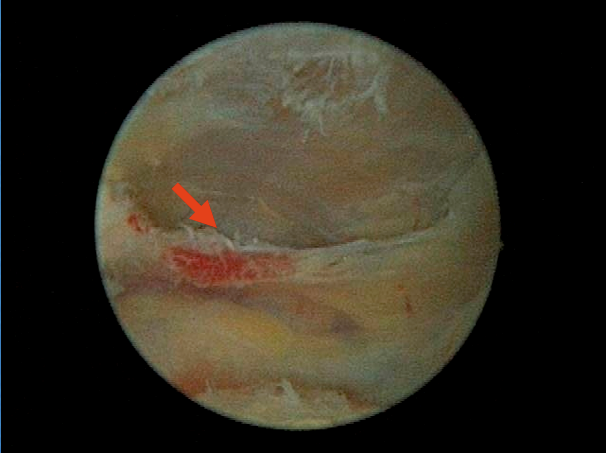
Even more narrowed knee joint space in X-ray, In arthroscopy, the cartilage surface has crumpled or abraded, appearing whisker-like.

Stage IV:
The joint space is almost all gone and bone spurs are obvious. In arthroscopy, some cartilage is completely worn off, and the bone underneath is exposed.
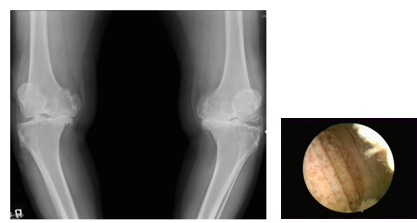
Stage V:
The joint space is all gone and bone spurs are obvious. In arthroscopy, all cartilage is completely worn off. Severe deformity has led the lateral ligament to become loose, unable to provide stability.
We recommend that all stages I and II and certain stage III patients undertake conservative treatment under medical supervision for at least three months. The patients and their families must completely understand the reasoning behind the conservative treatment in order for it to be successful.
We first emphasize that medial abrasion phenomenon is an important cause for osteoarthritis. Then we review the daily routine of a patient so we may discuss how, if anything, to modify his or her routine at home, on the job, or during workouts so as to minimize abrasion in his or her knee. In principle, movements that require repeated bending of the knee are harmful to the knee.
Table I is compiled based on this principle, Therefore, if your activity is not on this list, you can apply this principle to judge if it is knee friendly.
To avoid exerting shearing force harmful to cartilage regeneration, a recuperating patient should avoid repeatedly bending their knees more than 50 degrees. Therefore, sufferers of OA knees may engage in activities such as walking, jogging, golfing, and swimming freestyle or butterfly strokes. But they are advised to refrain from knee-damaging activities such as climbing up or down stairs, mountain climbing, squatting (such as gardening), bicycling, and swimming breaststroke.
Three recommended rehabilitation exercises under the KHPO
Like tooth brushing for oral hygiene, these rehabilitation exercises are recommended to be performed lifelong for the health of your knee.
| Suitable activities | Harmful activities |
|---|---|
| Walking | Climbing up or down stairs |
| Jogging | Mountaineering |
| Golfing | Repeatedly Squatting or kneeling (e.g. Gardening) |
| Freestyle swimming | Bicycling |
Three recommended rehabilitation exercises under the KHPO

A."Leg Raise" for quadriceps strengthening

B."Knee Press" for anterior soft tissue stretching

C."Knee Hug" for posterior soft tissue stretching
Rehabilitation and muscle strengthen training
The most economical, convenient, and effective methods:
- Strengthening the quadriceps: Raise leg and straighten the knee to strengthen the quadriceps, as in Diagram A.
- After each quadriceps exercise, slowly bend your knee to the limit and hold in the knee bend exercise, Diagram C, and straighten your knee and press, Diagram B, to maintain the range of motion of the knees and to reduce stiffness.
If you have received the ACRFP, we suggest that you work with trained personnel, such as case managers or specialized nurses, to monitor the training of the muscles around your knee joints and soft tissues and your at-home rehabilitation.
Download link:Download 1

Once we have staged a knee, we advise the patient to undergo a conservative treatment of exercises to strengthen and stretch out his or her quadriceps and soft tissues, respectively. We also advise the patient of the potential surgery, based on Table 3, that he or she may possibly be receiving.
For stages I, II, and III patients, Arthroscopic Cartilage Regeneration Facilitating Procedure (ACRFP) is a better treatment than knee replacement. For stage IV patients, knee replacement is typically the first choice, but when certain conditions exist, the ACRFP could be a very good choice.
| Stage | ACRFP | Microplasty of the knee | TKA (total knee arthroplasty) |
|---|---|---|---|
| I | + | - | - |
| II | ++ | - | - |
| III | +++ | ++ | - |
| IV | + | +++ | ++ |
| V | - | + | +++ |
In 2005, we developed a novel surgical procedure Arthroscopic Medial Release (AMR) to treat the medial abrasion syndrome.
As early as 1940, surgeons already severed the medial collateral ligament of the knee to treat knee OA with severe deformity, and papers were first published in 2001 about arthroscopic surgery to severe medial collateral ligament of the knee to treat knee OA. They attributed the therapeutic benefits simply to the reduction of pressure. However, those benefits did not last long and those arthroscopic surgeries did not catch on because those physicians did not know about the medial abrasion phenomenon which is an important cause of knee OA.
Unlike those arthroscopic procedures that merely severed the medial ligament indiscriminately, our Arthroscopic Medial Release procedure is precisely targeted to sever the third layer and a small part of the second layer (see the diagram) of the three-layer medial support structure in the knee.The capsulectomy extends superiorly to the midline of suprapatellar pouch. Inferiorly, it extends to the upper margin of medial meniscus. Anteriorly, it extends to the medial margin of patella. Posteriorly, it is undertaken to remove portion of the conjoined part of layer II and III till the gracilis tendon is visualized. Only the deep medial ligament was severed by this procedure and the medial stability should not be disturbed much.
Because only the deep medial ligament is severed, this procedure does not impact the stability of the knee.
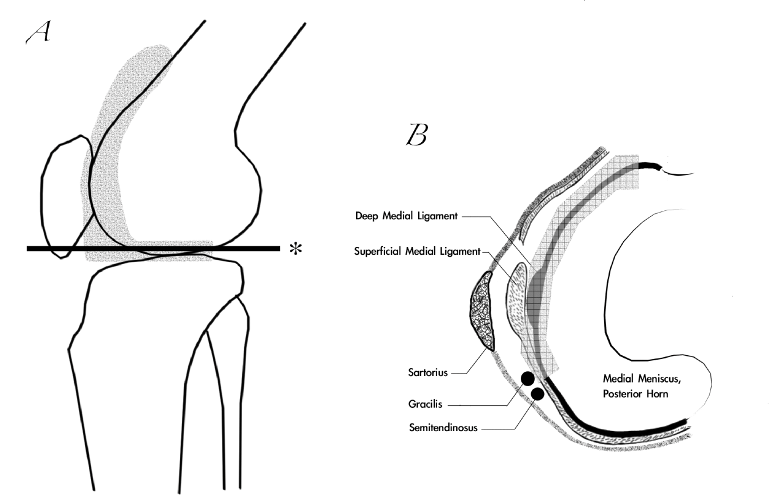
Diagram A:
The shaded area is the area excised in an AMR operation.The extent of the medial capsulectomy is shown in the hatched area of the line drawing of the lateral view of the knee joint. The line marked by * is the level of crosssection above the meniscus as shown in Diagram B.
Diagram B:
The arrowed area indicates the extent of the capsulectomy above the medial meniscus. Note that only the deep medial ligament is severed. The tendon of gracilis could be visualized after the procedure.
The adequacy of the medial release could be checked by passing the scope under the patella and verified if the previously tightly closed medial patellofemoral joint space could be easily opened and the medial retinaculum visualized when the knee was put in full extension position.
A

B

C

D

E

F

G
For a complete arthroscopic medial release (MAS), A, proximally, the genu articularis muscle attachment (arrow) should be released; B, the anterior synoviomeniscal junction (arrow) should be release; C, the medial gutter should be cleared to its posterior corner (arrow); D, the synoviomeniscal junction of the medial meniscus (arrow) should be clearly seen; E, in some case, release of the fascia of pes anserinus (arrow) should be performed; F, before medial release; G, after medial release.
According to our experience of performing this procedure (Lyu SR, 2008), the outcome of 255 knees in 173 patients for varying stages of osteoarthritis involving the medial compartment supports our contention that AMR is a good modality for the treatment of osteoarthritis of the medial knee joint in the aspect of symptom relief. It can reduce the pain in the majority of OA patients over a period of at least 4 years. In some cases, we also found the evidence that AMR could modify the disease process and satisfied the patients.
The clinical outcome of the AMR led us to believe that, by eradicating the abrasion phenomenon between the tight, fibrotic and hypertrophied medial plica related structure and the opposite medial femoral condyle, the pain of most patients could be reduced and the degenerative process in the medial compartment of some patients might be decelerated or arrested. Therefore, we propose a concept of arthroscopic cartilage regeneration facilitating procedure (ACRFP) that combines arthroscopic medial release (AMR) with synovectomy, abrasional chondroplasthy, partial meniscectomy or percutaneous lateral release (PLR) as a rationale for the deliberate arthroscopic management of OA knee. We believed that the elimination of the detrimental factors including the medial abrasion phenomenon, focal or generalized synovitis, chondral flaps, meniscus flaps or lateral compression phenomenon will provide a more hospitable environment for the damaged cartilage to regrow.
The ACRFP is built on a clear theoretic foundation and proven clinically. Its primary clinical objectives are:
- to remove all abnormal frictions, such as collagen fragments from damaged cartilage, and pinching phenomena, such as inflamed and thickened synovium, in the knee,
- adjust and release excessive tension between articular surfaces as a result of repeated inflammation of soft tissues over a long period so as to relieve articular surfaces of harmful pressure,
- remove all inflamed and thickened synoyium in the knee, which may cause cartilage to breakdown.
Proper execution of the ACRFP can improve the environment in the knee, making it more hospitable for cartilage to repair itself naturally.
Our surgical experiences, X-rays, and long-term follow-ups of patients have enabled us to be certain of this conclusion:
The ACRFP is an effective treatment for knee OA and it improves the course of this common disorder. If the existing catabolic factors in the knee joint have been thoroughly removed—which the KHPO does—the anabolic factors begin to take the lead in repairing the damaged knee. Then the damaged cartilage can regenerate and repair itself.
After the detrimental factors including medial abrasion syndrome, lateral compression syndrome, synovitis, chondral debris and meniscus flaps that have been proven as the main causes of cartilage damage are eliminated by ACRFP, the purpose of the post-operative care is to unveil and facilitate the natural repairing ability of the degenerated cartilage. During the first 3 months after ACRFP, the aim of rehabilitation is to prevent scar contracture and consequent recurrent medial abrasion phenomenon. Gentle deep bending stretching exercise is encouraged after each session of quadriceps strengthening exercise. To facilitate cartilage regeneration, strict rules about engaging into appropriate daily activities and exercises as listed in table 3 should be followed during the first post-operative year. The rationale of this precaution is to avoid repeated bending of the knee that might produce shearing force harmful for cartilage regeneration. Patients are advised to do muscle strengthening and soft tissue stretching exercises around the knee for as long as possible.
The PCRFM includes:
Rehabilitation exercises. These are the most economical and efficient method.
- the exercise to strengthen the quadriceps by extending the leg (diagram A).
- During the three months after the ACRFP, the objectives of rehabilitation is to prevent scarring on the wound, which could bring about the recurrence of the medial abrasion phenomenon, Therefore, each time after you have finished your quadriceps exercise, you must also do both press knee, (B), and knee hug, (C).
- To promote cartilage regeneration, you are advised to observe and do only exercises that are listed in Table 3, exercises that do not bend the knee repeatedly and possibly create frictions that hinder the re-growth of cartilage. Walking is the most convenient and effective exercise. It also helps keep your weight down.
- One year after the ACRFP, if appropriate, you may gradually return to your own original routine.
- These three exercises help prevent cartilage from being damaged again. Therefore, if at all possible, you are advised to keep doing them forever.

A.Leg Raise for quadriceps strengthening

B.Knee Press for posterior soft tissue stretching

C.Knee Hug for anterior soft tissue stretching
Medical establishments elsewhere have promoted external therapies that claim to stimulate the growth of cartilage. These methods are more costly but offer uncertain results. Some studies have shown these methods to suppress inflammation, and PRP has been shown to facilitate the anabolism of cartilage and enhance its ability to repair itself. Perhaps they deserve a closer look.
Overall, 94.1 percent of our patients have been satisfied with the KHPO
After one year, 511 patients with 844 affected knees (97.9%) remained enrolled in the study. The mean age of these patients at the time of surgery was 64 years (SD: 10). Subjective assessment was satisfactory in 794 (94.1%) knees. Six-hundred-and-fifty-seven knees (77.8%) of 379 patients received an arthroscopic cartilage regeneration facilitating procedure (ACRFP), 71 knees (8.4%) of 70 patients received unicompartmental arthroplasty (UKA), and 116 knees (13.8%) of 116 patients received total knee arthroplasty (TKA). For the arthroplasty group, the subjective assessment was satisfactory in 187 knees (100%). For the ACRFP group, the subjective assessment was satisfactory in 607 knees (92.4%). In the ACRFP group, the satisfactory rate was 91.2% for 228 stage II knees, 93.6% for 327 stage III knees, and 91.2% for 102 stage IV knees. Three knees in the stage IV group had converted to arthroplasy after the minimum follow-up of one year.

It is thrilling to see patient satisfaction as high as these.
Even our stage IV patients, who would have been treated with TKA or uni-K under the conventional treatment protocol, have benefited from the ACRFP treatment: They have gotten relief from their OA symptoms without giving up their natural knees, and they are still satisfied with the ACRFP--and their knees--three years after the treatment.
The difference in satisfaction among patients in stages II, III, and IV suggests that it is advisable to get the ACRFP treatment as early as possible.
Although articular hyaline cartilage was typically considered as having no or low potential for regeneration (Zhang L et al., 2009), some researchers still thought that it does have the capacity to grow, and they remodel extensively during pre- and post-natal development and after trauma (Onyekwelu I et al., 2009). Both direct and indirect evidence of articular cartilage regeneration after correction of varus deformity for osteoarthritis of the knee has been observed by some authors (Kanamiya T et al., 2002; Koshino T et al., 2003).
Moreover, despite the typical image of a largely static tissue, articular cartilage does show a turnover, albeit slowly. Anabolic and catabolic pathways were thought to be very much intermingled in articular cartilage (Aigner T et al., 2006). Thus, one of the most important issues in osteoarthritis research is to understand the interaction and balance between the catabolic and anabolic factors in articular cartilage because this is the key to understanding the biology of cartilage maintenance and degeneration.
In 2006, we reported that in patients with medial compartment osteoarthritic knees, the prevalence of medial plica was significantly higher than that of others and that two distinct foci of cartilaginous lesion were found on the facing medial femoral condyle in almost all of the patients who had the structure of medial plica (Lyu SR and Hsu CC, 2006). Our further study disclosed the kinematic relationship of the medial plica with the medial femoral condyle during knee motion in vivo (Lyu SR, 2007). In that study, it was revealed that all medial plicae, regardless of their size, would move reciprocally and would keep in touch with the medial femoral condyle and therefore might cause some degree of abrasion on the facing medial femoral condyle during knee motion. Another histomorphological study of the medial plica also implied the close interplay between this structure and the medial femoral condyle (Lyu SR et al., 2009). Moreover, our recent study (Wang HS et al., 2011)
Osteoarthritis – Diagnosis, Treatment and Surgery 380 found that the repeated injuries elicited by this abrasion phenomenon might trigger interleukin-1 (IL-1) production in medial plica, thus enhance the expression of matrix metalloproteinase-3 (MMP-3). Based on these findings, we developed a concept of arthroscopic medial release (AMR) for the treatment of osteoarthritis of the medial compartment of the knee joint (Lyu SR, 2008).
The clinical outcome of this procedure led us to believe that, by eradication of the abrasion phenomenon between the tight, fibrotic and hypertrophied medial structure and the adjacent medial femoral condyle, the pain of most patients could be reduced and the degenerative process in the medial compartment of some patients might be decelerated or arrested. Recently, we proposed a concept of arthroscopic cartilage regeneration facilitating procedure (ACRFP) that combines arthroscopic medial release (AMR) with conventional arthroscopic procedures including synovectomy, chondroplasty, partial meniscectomy and percutaneous lateral release (PLR) as a rationale for the deliberate arthroscopic management of OA knee. We’ve found that the elimination of the existing detrimental factors will provide a preferable environment for regeneration of the damaged cartilage.
The following exhibits illustrate the ability of cartilage to regenerate:

A

B
The medial compartment of the left knee of a 56-year-old woman with stage II OA;
- A, cartilage erosion was found over the medial femoral condyle opposite the pathologic medial plica which we had removed during an ACRFP procedure;
- B, during the second-look arthroscopy 3 years later when the same knee suffered from hemoarthrosis after suffering a fall, we visualized the eroded cartilage at this defect site to have regenerated.

A

B

C
A self-control example showing the benefit of ACRFP:
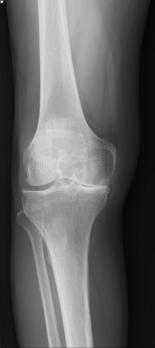
- A, pre-operative AP standing view of a 61-year-old male with stage III knee OA over the medial compartment of the right knee and stage II knee OA over the medial compartment of the left knee. ACRFP was performed for his right knee;
- B, 46 months later, he came back to us for his marked disability in his left knee (untreated with ACRFP and was now severely deformed). His ACRFP-treated right knee, however, was in excellent condition and was showing that the degenerative process had ceased (as compared with his left knee, which was still progressively degenerating)
- C, unicompartmental arthroplasty was necessary for his left knee that hadn’t received ACRFP.

A

B
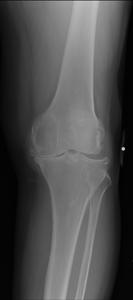
An example of reversal of natural degenerative course by ACRFP in a 70-year-old male patient having stage IV knee OA over his right knee:
- A, pre-operative standing AP view showing stage IV knee OA over the medial compartment of his right knee;
- B, three years after the ACRFP, the joint space had reopened and the FTA had improved from 7 degrees varus to 3 degrees varus.

A

B
Another example of reversal of degeneration after the ACRFP treatment:
- A, AP standing view of a 58-year-old female patient having bilateral stage IV knee OA with subluxation of medial femoral condyle;
- B, three years after the ACRFP, obvious improvement of the radiographic manifestation could be observed.

A

B
The ACRFP and high tibia osteotomy reverse degenerative knee OA for a 58-year-old female patient.
A.An AP standing view shows stage IV knee OA that has resulted from the malunion of an old fracture. The knee shows marked improvement two years after receiving the ACRFP and high tibia osteotomy.

Related links:Precision Arthroplasty
Even before reaching late-stage knee OA, a patient's articular surface may have already severey worn off or deformed, leading to pain, restricted mobility or other function, and diminished quality of living. Arthroplasty can markedly relieve symptoms, correct deformity, and effectively improve knee function, so it is the fastest and a relatively effective method to treat knee problems. It has helped countless mobility-restricted patients. In Taiwan, patients of severe knee OA receive arthroplasty more than 20,000 person times each year. There are two types of arthroplasty:Microplasty of the knee and total knee arthroplasty.
Microplasty of the knee
This arthroplasty, diagram 1, is used when only one articular surface is damaged. The surgery is analogous to filling a dental cavity. While total knee arthroplasty removes all tissues in the knee, unicompartmental arthroplasty needs to fix the damaged articular surface and thus keep normal tissues in tact. Ergonomically designed mobile disk, which is covered by the femur, allowing bigger range of motion like a ball. This design causes less abrasion resulting from friction on a single point than does a design of fixed knee joint. Patients recover faster. Physiological functions, which almost mimic a natural knee, can return to almost normal levels.
However, constrained by the small incision, the surgeon needs to perform such acts as cutting and grinding bones in a small space. Therefore the surgeon needs to possess a higher level of surgical dexterity, expertise, and experience in order to perform Uni K.
Diagram 1
Pre-surgery

Prosthesis

Post-surgery
Precision Arthroplasty
Precision Arthroplasty, also known as TKA, is the most common form of knee replacement surgery. It is suitable when the patient suffers severe deformity or more than two articular surfaces are damaged.
The procedure excises damaged articular surface, smoothes out the area, and installs the prosthesis to enable the knee to move smoothly and to correct deformity. TKA is analogous to dental implant.
TKA unavoidably excises and damages tissues. For example, the anterior cruciate ligament, posterior cruciate ligament, and meniscus in the knee are all excised. Consequently, a patient with an artificial knee cannot move as naturally and freely as before.
Diagram 2
Pre-surgery

Prosthesis

Post-surgery
Arthroplasty offers high success rates and apparent and immidiate improvement, but serious complications are occasionally possible. Therefore, the patient must be very clear before deciding to undergo this treatment. They should be fully aware that arthroplasty is the last resort of all treatments for knee OA and that once the procedure is performed, there is no going back whatsoever. All patients should take utmost care before proceeding.

- avoid these exercises or movements: stairs climbing, mountain climbing, bicycle riding, breaststroke, squatting, kneeling, and sitting with knees bent for long periods.
- do these exercises: walking, freestyle, or water walking.
If conservative treatment does not help alleviate symptoms or your cartilage continues to erode, then you may be assessed for suitability for the ACRFP in order to eradicate risk factors for knee OA and to give your knee an opportunity to regain function.
A.The traditional arthroscopic surgery: It debrides or drills bones indiscriminately with no specific targets. Reputable professional societies have clearly declared that this arthroscopic surgery is ineffective in the treatment of knee OA and that they are against this procedure.
On the contrary, our ACRFP is built on solid research that spanned over a decade. Each ACRFP is tailored to meet the need of the knee in question, so an ACRFP can be a combination of the Arthroscopic Medial Release (AMR, always performed) and none, some, or all of the following procedures: Arthroscopic Partial Meniscectomy, Arthroscopic Synovectomy, Arthroscopic Loose Body Removal, and Arthroscopic Chondroplasty. The ultimate goal of the ACRFP is to erase all abnormal abrasion and inflamed tissues by (a) excising the medial plica, (b) removing inflamed and thickened medial synovium and capsule, and (c) adjusting and fine tuning the tension between patella and femoral condyle--to leave cartilage an environment that is most hospitable and anabolic to its regeneration.
- The ability to perform arthroscopic surgery, particularly the ability to operate in the tight space in a knee cavity.
- Study from and observe the surgeries of a qualified surgeon and have three to five years of experience.
- Fully understand and endorse the concept of the Knee Health Promotion Option so as to be able to lead a team to use this concept to treat and educate patients. This aspect seems to be particularly challenging for surgeons to comply with because the concept is not taught in medical school. The more senior a surgeon already is, the more difficult for him or her to adapt the KHPO.
Our training program has set a minimal success rate as for every 100 cases treated, at least 80 patients are satisfied at least one year after the procedure.
1.The first month after surgery is for the wounds to heal.
- The swelling and bruise gradually fade. The wounds still hurt, but it is a different kind of sensation than the pain before surgery. Overall, the knee feels much more comfortable than before surgery. Uncomfortable symptoms like tightness and soreness greatly diminish.
- The overriding objective of self care during this stage is to protect the wounds so they may heal smoothly. So do the following exercises gradually and gently, never to hurt the wounds.
- Three rehab exercises: leg raise, knee hug, and press knee
- Activity: walking on level grounds, but for a distance that does not cause knee pain.
2.The first month after surgery is for the wounds to heal.
- The process of fibrosis gradually developing in healed wounds is most apparent in the second and third months after surgery. This is why doing the three daily rehab exercises is so important. Not doing these exercises diligently every day allows tightness and soreness to return. The patient may feel frustrated and wrongly blame the discomfort on the ACRFP. In fact, fibrosis and subsequent tightness and soreness are a normal part of the healing process. Therefore, the daily rehab exercises must be done diligently every day in order to counter the effects of fibrosis.
- The overriding objective in this stage is to strengthen the muscles and to prevent excess fibrosis from forming in the scars. Since the wounds are already healed, they can take some pain. Therefore, it is strongly suggested that you do the rehab exercises in spite of the pain, every day. You must persevere. The pain you suffer during the exercise now will pay you back in the form of painless days in the future
- Three rehab exercises: leg raise, knee hug, and press knee
- Activity:Increase the distance of your walks. You may resume light work. Refrain from taking stairs up or down, carrying heavy things, squatting, kneeling, and sitting for long periods of time with knees bent.
3.From the fourth month to one year after surgery is when the wounds stabilize and the cartilage repairs itself.
- Fibrous tissues (scars) gradually soften. By and large, the knee gradually feels more and more comfortable except some minor nerves near the wounds that may cause pain and sensitivity.
- The overriding objective during this stage is to strengthen the muscles and to protect cartilage, which is repairing itself.
- Three rehab exercises: leg raise, knee hug, and press knee. Localized massaging may help diminish the sensitivity around the wounds.
- Activity:Increase the distance of your walks on level grounds. You may resume your normal activities. To protect the self-repairing cartilage, you should continue to refrain from taking stairs up or down, carrying heavy things, squatting, kneeling, and sitting for long periods of time with knees bent.
4.One year after surgery is when cartilage repairs itself and function returns to normal.
- The factors in the knee that are detrimental to the normal metabolism of cartilage have been completely removed by ACRFP, so the knee now offers a hospitable environment in which cartilage may function normally and repair itself. You need only to continue the daily rehab exercises, and your knee will get better with time.
- Three rehab exercises:leg raise, knee hug, and press knee. These three easy exercises are to healthy knees what brushing is to healthy teeth. Ideally, you should do them every day for life.
- Activity:As you gradually return to normal, you may gradually resume your normal activities and return to a healthy life.
Generally, if a patient receives the ACRFP before the knee has deteriorated beyond repair (severe deformity) and follows the surgery with appropriate rehab exercises, then he or she can reasonably expect improvement.
Therefore, it is apparent that the ACRFP delivers much more blood to the knee cavity. If you really want to consider getting PRP injections, we recommend that you wait at least a year after you have received the ACRFP. A follow-up at that time will give you and your doctor an opportunity to assess whether or not it makes sense for you to get a PRP shot.
We have seen patients whose symptoms worsened after they had been treated with traditional arthroscopy. The reason for that deterioration was clear to us: Their surgeons did not know about and hence did not address the medial abrasion syndrome when they performed the arthroscopy. Therefore, their operations caused severe scarring of tissues. This situation can be made better with the ACRFP under the KHPO.